The examination of an orthopedic-traumatological patient is based on general clinical methods, but the specifics of orthopedic conditions and the clinical features of traumatic injuries require additional knowledge and approaches. Diagnosing such conditions is a complex cognitive process consisting of several sequential stages. The physician must follow a clear sequence and a pre-determined examination plan.
The clinical examination techniques used to identify symptoms of the disease and establish a diagnosis include the following stages:
- Determining the patient’s complaints: It is important to establish the nature, intensity, location, and duration of pain or other symptoms.
- Medical history of the disease (trauma): This includes details about the circumstances of the injury or disease onset, symptom progression, and any prior treatment, if such was provided.
- Life history: Previous diseases, surgeries, genetic predispositions, and risk factors that could influence the development of musculoskeletal pathology are assessed.
- Patient examination: A visual assessment aimed at identifying deformities, swelling, pathological changes in the limbs, skin color changes, or other visible abnormalities.
- Palpation: This helps detect painful areas, the presence of swelling, muscle atrophy, or other pathological changes in the soft tissues.
- Range of motion assessment in joints: Both active (performed by the patient independently) and passive (performed by the physician) movements are evaluated to determine potential limitations or deviations from normal.
- Muscle strength evaluation: This allows for the detection of possible weakness or atrophy, which may be the result of neuromuscular disorders or injuries.
- Measurements: Length of limbs, joint volumes, and muscle circumferences are measured to compare with the contralateral side or normative values.
- Joint function assessment: The general functional ability of the joint is evaluated, including its stability, range of motion, and capacity to bear weight.
Before collecting complaints, it is important to familiarize oneself with the passport section of the patient's medical history. Since certain orthopedic conditions are directly related to age characteristics, this can help the physician consider or rule out specific pathologies early in the examination process.
PATIENT COMPLAINTS
When carefully listening to a patient's complaints, it is important for the physician to distinguish between primary and secondary issues. In typical clinical practice, patient complaints usually involve pain, loss, or dysfunction of the musculoskeletal system, as well as cosmetic concerns (e.g., the presence of deformities). Pain is a key signal indicating the presence or threat of a disease. In orthopedic practice, patients may not always be able to precisely define their concerns, as the combination of various deformities may have varying degrees of intensity. There are cases where secondary changes bother the patient more than the primary pathology, leading them to focus on these.
In cases of multiple injuries, patients often complain about the most painful areas, even if this is not the most severe injury. If the physician overlooks this and fails to conduct a thorough examination, serious consequences may result.
MEDICAL HISTORY
Taking a detailed medical history provides valuable information directly related to the disease and the overall characteristics of the patient. It allows the physician to determine when the first symptoms appeared, the circumstances of their onset, as well as the influence of external and internal factors (e.g., physical exertion, temperature conditions, and the effectiveness of previous treatments). The medical history also gives the physician insight into the patient’s personality, lifestyle, working conditions, and prior illnesses.
For congenital malformations, special attention must be given to genetic factors and the conditions during the mother's pregnancy. It is essential to differentiate between endogenous (genetic) and exogenous (teratogenic) factors. The former arise from pathological changes in the genes inherited from parents, while the latter are due to the impact of harmful agents during pregnancy (e.g., chemical, radiation, or infectious factors).
The history of inflammatory diseases should clarify the nature of the process (acute or chronic), the temperature curve, the duration of the acute phase, whether the lesions are multiple or isolated, the presence of changes in other organs, and the effectiveness of previous treatment.
The history of degenerative processes requires an assessment of the characteristics of the disease course, as pain that occurs during exertion may subside during rest. It is crucial to determine the duration of the condition and the extent of anatomical and functional changes.
The history of traumatic injuries requires a detailed investigation of the injury mechanism (direct or indirect). Important details include the angle and direction of the force causing the injury, the patient's position at the time of the injury, and the circumstances under which the accident occurred (e.g., workplace, domestic, or sports-related injury). For open injuries, it is necessary to establish the place, time, and circumstances of the injury, as well as the quality of the first aid provided.
PATIENT EXAMINATION
The examination of an orthopedic-traumatological patient follows general clinical requirements (comfortable temperature, adequate lighting, and the patient being undressed) but also has its own specifics. The patient is examined in various positions: standing, sitting, lying down, and during movement. The physician evaluates height, body and limb proportions, posture, gait, and assesses active, passive, and forced body positions.
- Active position: The position the patient assumes independently, moving freely, getting out of bed, or moving around the room.
- Passive position: The state when the patient cannot change position independently due to the severity of the disease (e.g., head injury, coma, nerve damage).
- Forced position: Often caused by pain or morphological changes in tissues (e.g., ankylosis, contractures, dislocations). Pathological postures may occur as compensatory changes, distant from the primary site of injury. For example, shortening of a limb after a fracture may lead to pelvic tilt, spinal curvature, and limping.
Vertical Position Examination
Thanks to compensatory spinal curvatures, body mass is evenly distributed between the anterior and posterior parts, as well as symmetrically between the right and left halves of the body. This is achieved through the symmetry of body structure.
Three reference planes are used to assess the spine, shoulder, and pelvic girdle positions, and the distribution of body mass. These planes are mutually perpendicular to each other.
These planes are based on the position of the body’s center of gravity, located at the level of the second sacral vertebra. The first plane passes through the center of gravity in the horizontal direction and is called the horizontal (transverse) plane. At a right angle to this is the sagittal plane, which divides the body into right and left halves. The third plane, the frontal plane, is perpendicular to the previous two and divides the body into anterior and posterior halves.
When examining the patient, attention is given to the position of the torso, limbs, and head relative to these reference planes, i.e., posture is assessed.
Posture refers to the vertical position of the body developed throughout life, which maintains the physiological curves of the spine, the symmetrical position of the head, shoulder girdle, and upper and lower limbs, as well as the horizontal position of the pelvis (see Fig. 1 a, b).
Posture Assessment
When examining posture, special attention is paid to the shape of the back, which can take several characteristic forms:
1. Harmonious back: The physiological curves of the spine are preserved—cervical and lumbar lordosis, as well as thoracic and sacral-coccygeal kyphosis.
2. Flat back: The physiological curves of the spine are flattened, with the cervical lordosis remaining intact.
3. Stooped back: There is an increased thoracic kyphosis, and the lumbar lordosis is flattened. The shoulder girdle is shifted forward, the chest is flattened, and the shoulder blades protrude like "wings."
4. Round-concave back: The pelvis is significantly tilted forward, leading to an increased lumbar lordosis and a compensatory increase in thoracic kyphosis.
5. Scoliotic posture: There is a curvature of the spine in the frontal plane, without rotation or torsion of the vertebral bodies.
Gait Examination
Limping is a gait disturbance characterized by alterations in movement rhythm due to vertical swaying of the body. There are two main types of limping:
1. Protective (painful) limping: The patient avoids fully loading the affected limb due to pain. They protect the limb during walking, placing weight on it only briefly and often using assistive devices.
2. Non-protective limping: Observed in cases of limb shortening or ankylosis and is not accompanied by pain.
Several typical gait disorders are identified:
- "Waddling" gait: The trunk sways from side to side. This is seen in bilateral congenital hip dislocation or bilateral pathology such as coxa vara.
- "Hopping" gait: Occurs due to leg lengthening.
- "Diving" gait: The trunk sways to one side, observed in unilateral congenital hip dislocation.
- Paralytic gait: Seen with isolated paralysis or paresis of individual muscles.
- Spastic gait: Characterized by increased muscle tone, typical for spastic paralysis.
Local Examination
The examination of the skin and mucous membranes is an important part of the local evaluation. Changes in skin color, the presence of hemorrhages, their location, and extent are assessed. To do this, transport immobilization is carefully removed, and the patient is partially or fully undressed.
Particular attention is paid to:
- The nature of the inflammatory reaction along the lymphatic vessels, veins, and tendons;
- The presence of epidermal vesicles (blisters) with soft tissue edema;
- Hematomas, scratches, wounds, fistulas, scars;
- Swellings, edema, changes in skin tension, paleness, or the appearance of a venous network.
Examination of Limbs
To obtain complete information about the condition of the limbs, the examination follows a specific sequence. It is always comparative and segmental. First, general changes that disrupt the anatomical structure of the limb are assessed, then the injured area is examined, and the evaluation concludes with an assessment of changes in the segments above and below, focusing on muscle condition and compensatory changes.
Severe disruptions include:
1. Pathological joint positions.
2. Changes in the normal axis of the limb.
3. Disruptions in the mutual positioning of the joint segments.
Pathological joint positions arise due to joint disease or its consequences (contractures, ankylosis), as well as from extra-articular changes. The limb or its segments can become fixed in certain positions, such as:
- Genu flexum: Flexion deformity of the knee joint.
- Pes equinus: Equinus deformity (plantar flexion of the foot).
- Genu recurvatum: Hyperextension of the knee joint.
- Cubitus antecurvatum: Hyperextension of the elbow joint.
- Crus antecurvatum: Forward angular deformity of the tibia or thigh.
- Crus recurvatum: Backward angular deformity.
Fig. 2
Determination of the Axes of Normal Limbs
The axes of normal limbs are determined using auxiliary lines drawn in the frontal plane when the limbs are in their physiological position.
The clinical axis of the lower limb passes through the following landmarks:
- the anterior superior iliac spine (spina iliaca anterior superior),
- the medial border of the patella,
- the first interdigit space (see Fig. 3).
In the absence of lateral curvatures, all three of these points should lie on a straight line. Any deviation of these points from the straight line indicates a deformation of the limb axis.
The axis of the upper limb passes through the following landmarks:
- the head of the humerus,
- the head of the radius,
- the head of the ulna (see Fig. 4).

Fig. 3. Fig. 4.
Changes in the Normal Limb Axis
Changes in the normal limb axis occur with lateral curvatures, which may develop either at the joint or along the diaphysis of the bone.
- Varus deformity (O-shaped deformity) occurs when the limb segments are displaced outward from the normal axis, creating an inward-facing angle (see Fig. 5a).
- Valgus deformity (X-shaped deformity) appears when the limb segments are displaced inward from the axis, and the angle between them opens outward (see Fig. 5b).
Fig. 5a Fig. 5b
Identification of Possible Congenital or Acquired Foot Deformities
For a practicing physician, it is important to identify possible congenital or acquired foot deformities, which include:
- Valgus foot: The foot deviates outward from its normal axis.
- Varus foot: The foot deviates inward from its normal axis.
- Equinus foot (pes equinus): The foot is fixed in a plantar flexion position.
- Calcaneus foot (pes calcaneus): The foot is fixed in a dorsiflexion position.
- Cavus foot (pes cavus): The foot arch is excessively elevated.
- Flat foot (pes planus): The foot arch is lowered, leading to flatfoot.
Joint Misalignment
Depending on the nature and degree of changes, joint misalignments are categorized as:
- Dysplasia (displasia): This is an underdevelopment of the joints where the correct alignment between joint surfaces is preserved. However, due to underdevelopment of one or both meta-epiphyses, the normal contact between joint surfaces is disrupted.
- Subluxation (subluxatio): A partial disruption of the congruence (alignment) between joint surfaces.
- Dislocation (luxatio): A complete disruption of the congruence of joint ends. Typically, dislocations and subluxations are named after the peripheral segment of the limb (e.g., shoulder or foot dislocation). An exception is made for vertebral and clavicular dislocations, where the dislocated segment is directly indicated (e.g., dislocation of the sternal end of the clavicle).
Dislocations are classified as congenital or acquired. Acquired dislocations are further divided into traumatic, pathological, and paralytic, with habitual dislocations also existing.
- Traumatic dislocations involve displacement of the joint surfaces, accompanied by a tear of the joint capsule, ligament damage, and muscle synergy disruption, resulting in the typical clinical symptom of elastic fixation. The direction of dislocation can be posterior, anterior, superior, inferior, or lateral.
- Pathological dislocations often result from inflammatory processes and are divided into:
- Distensive dislocations: Occur due to inflammatory effusion, leading to displacement of joint surfaces caused by reflex muscle tension, without bone destruction.
- Destructive dislocations: Occur with significant destruction of joint surfaces and simultaneous changes in surrounding soft tissues (e.g., tuberculosis, tumors, osteomyelitis).
- Paralytic dislocations: Seen in flaccid or spastic paralysis, myopathies. These are caused by disturbances in muscle tone and synergy.
Examination of Joints and Limb Segments
Joint swelling is observed in para-articular edema, bursitis, tendon sheath edema, and intra-articular pathologies such as hemarthrosis or effusion. Tumors can deform the joint, giving it an irregular, nodular appearance.
During limb segment examination, attention is focused on:
- Protrusions and deformities.
- Pathological mobility.
- Muscle development and atrophy.
Palpation
Palpation is used both for general patient assessment and for examining localized lesions. General palpation follows standard guidelines and includes examination of the abdominal organs, pelvis, lymph nodes, and evaluation of muscle tone.
The physician visually monitors the process during palpation. Palpation is performed both at rest and during patient movements. The palpation of anatomical landmarks follows a specific sequence—from top to bottom and symmetrically.
During localized examination, palpation provides important data:
1. Changes in local temperature—assessed by touching the affected area of the joint or limb with the back of the hand.
2. Localized tenderness—assessed by gentle pressure. In some cases, localized tenderness is the only clinical symptom. Palpation helps objectify pain syndrome (its nature, duration, radiation, especially with axial load).
3. Skin condition—skin mobility over the affected area is assessed, as well as skin fold thickness, the presence of subcutaneous abscesses, hematomas, edema, or subcutaneous tissue induration.
- Alexandrov's symptom: Thickening of the skin fold due to toxic edema of subcutaneous tissue in bone and joint tuberculosis. To detect this symptom, one hand is placed on the affected limb and the other on the healthy limb to compare the thickness of the skin fold.
4. Palpatory assessment of joint ends and bony prominences—palpation helps detect displacement of bony prominences or joint ends, allowing the evaluation of bone displacement. Joint palpation can also be performed during movement.
To determine correct anatomical relationships in joints, primary anatomical landmarks are used:
- Hunter’s triangle: Formed by points located at the tips of the humeral condyles and the olecranon when the forearm is flexed at a right angle. Normally, the triangle is isosceles (see Fig. 6a).
- Lines and triangles for joint injury diagnosis: For example, Mark’s, Schemmaker’s, and Roser-Nelaton’s lines and triangles are used for diagnosing elbow and hip joint injuries.
Gunther’s Line
In the extended position of the upper limb, the medial and lateral epicondyles, as well as the tip of the olecranon, are aligned on the same straight line (see Fig. 6b).
Mark’s Line
When the upper limb is flexed at the elbow joint at a 90-degree angle, the axis of the humerus forms a right angle with the line connecting the humeral epicondyles (see Fig. 6c).
Fig. 6b Fig. 6c
Bryant’s Triangle
Bryant’s triangle is formed by lines connecting the apex of the greater trochanter with the anterior superior iliac spine, and a perpendicular dropped from the anterior superior iliac spine to the extension of the longitudinal axis of the femur in the inguinal region (see Fig. 7a).
Roser-Nelaton Line
The Roser-Nelaton line connects the ischial tuberosity with the anterior superior iliac spine. Normally, when the lower limb is flexed at the hip joint at a 135-degree angle, the apex of the greater trochanter is located along this line (see Fig. 7b).
Roser-Nelaton Line in Fractures or Dislocations
In cases of femoral neck fractures or hip dislocation, the apex of the greater trochanter may be positioned either above or below the Roser-Nelaton line.
Shoemaker’s Line
Shoemaker’s line connects the apex of the greater trochanter with the anterior superior iliac spine. Normally, its extension passes through or slightly above the navel (see Fig. 8a).
Shoemaker’s Line in Cranial Displacement of the Greater Trochanter
When the greater trochanter is displaced cranially, Shoemaker’s line will pass below the navel (see Fig. 8b).
5. Tendon, Bursa, and Peripheral Nerve Assessment
The assessment of tendons, bursae, and peripheral nerves involves checking tendon mobility or adhesion to surrounding tissues, evaluating the size and thickening of bursa walls, and testing the sensitivity of nerve trunks to pressure.
6. Detection of Synovitis or Hemarthrosis
In the presence of effusion or blood in the knee joint, the patellar ballotment test can be used to identify the condition through palpation. Normally, when the limb is extended, the patella lies close to the anterior surface of the femoral condyles, but when there is excess fluid in the joint, the patella moves away from the condyles.
To diagnose effusion in the knee joint, with the limb in extension, one hand pushes the fluid from the suprapatellar pouch, while the fingers of the other hand press the patella, pushing it into the fluid until it contacts the femoral condyles (see Fig. 9a). After releasing the pressure on the patella, it rises back up, indicating the ballotment sign (see Fig. 9b).
Fig. 9b
7. Identification of Pathognomonic (Specific) Symptoms of Musculoskeletal Injuries
Specific symptoms of injuries include, for example, Baikov’s symptom and Steinman’s symptom, both used in examining the knee joint.
8. Palpation During Surgical Procedures
Palpation can be performed using the entire hand, fingertips, or both hands simultaneously (bimanual palpation). For more detailed palpation, a button probe can be utilized.
Auscultation
Auscultation has limited application in examining the musculoskeletal system. It is performed during passive movements of peripheral limb segments. In children and young individuals, joint movements are usually silent. In middle-aged and elderly individuals, slight crepitus may be noted, and in pathological cases, a characteristic crunch can be detected.
Range of Motion (ROM) Assessment in Joints
Both active and passive joint movements are evaluated. Passive movements may be unrestricted, while active movements can be limited or absent. The assessment begins with the determination of active movements, which are dictated by the anatomical structure of the joint. Results are recorded by measuring the range of motion with a goniometer. The arms of the goniometer are aligned along the axes of the segments forming the joint and move with them. The axis of rotation of the goniometer must coincide with the axis of movement of the joint. Measurements are taken from the neutral (zero) position.
Neutral (zero) position: The patient stands straight, looking forward, arms hanging freely along the sides, thumbs pointing forward, feet together, and parallel. This position can also be replicated in the lying position.
Movement directions:
- Sagittal plane: Flexion and extension (flexion-extension). For the foot and hand—plantar and dorsal (foot) or palmar (hand) flexion.
- Frontal plane: Abduction and adduction (abduction-adduction). For the hand—radial and ulnar movements.
- Longitudinal axis: External and internal rotation.
Measurement results using the neutral (0°) method are recorded in three figures: the central 0° represents the neutral position, with the extension, abduction, and external rotation values recorded before 0°, and flexion, adduction, and internal rotation values after 0°. Results for the right and left sides are recorded separately for comparison.
If the movement does not reach the neutral position, 0° is placed before or after the numeric values (for example, with an abduction contracture, flexion may not reach 0°, and the recording will be: 25°/15°/0°).
Spinal Movement Assessment
The neutral position for the torso is when the patient stands straight with even weight distribution on both legs, looking forward horizontally, and arms hanging freely at the sides.
- Cervical spine:
- Head tilt: flexion-extension (35-45°/0°/35-45°).
- Lateral head tilt (45°/0°/45°).
- Head rotation to the right-left (60-80°/0°/60-80°).
A special goniometer is used to measure movements in the cervical spine.
- Thoracic and lumbar spine:
- Lateral flexion (20°/0°/20°).
- Flexion-extension (40°/0°/30°).
In the thoracic and lumbar regions, forward flexion is measured using the floor-to-finger method—the distance from the floor to the patient’s fingers is noted.
Schober’s Method for Spinal Mobility Measurement:
- Mark the C7 spinous process.
- The second point is marked at the spinous process located 30 cm caudal to the first point (see Fig. 10a). When bending forward, a normal spine extends by 8 cm (see Fig. 10b).

Fig. 10a Fig. 10b
When assessing the lumbar spine, points are marked at the spinous processes of the L1 and L5 vertebrae. Normally, when the trunk flexes forward, the distance between these points increases by 4-6 cm. The obtained data are recorded as follows: thoracic spine mobility — 30 cm/36 cm, lumbar spine mobility — 10 cm/15 cm.
Upper Limb Mobility Assessment
Movement Assessment in the Shoulder Girdle
- Abduction-Adduction of the arm in the frontal plane: 180°/0°/20-40° (abduction beyond 90° is achieved through external rotation and scapular movement) (see Fig. 11a, b, c).
External-Internal rotation of the shoulder with the elbow flexed: 40-60°/0°/95° (see Fig. 13a, b).
Abduction/Adduction in the horizontal (transverse) plane: 90°/0°/45° (see Fig. 14a, b).
Movement Assessment in the Elbow Joint
The range of motion in the elbow joint is 140-155°. In women and children, this range may be greater due to hyperextension at the elbow joint. Rotational movements occur as the radius rotates around the ulna within a range of 180°, from full supination to full pronation. In the elbow joint, extension-flexion is 10°/0°/150° (see Fig. 15a, b).
In the radioulnar joint, pronation-supination ranges from 80-90°/0°/80-90° (see Fig. 16a, b, c).
Fig. 16a
|
Fig. 16b, c
Radial-Ulnar deviation ranges from 20°/0°/30°, with a total amplitude of 50° (see Fig. 17a, b, c).
Hand Grasps (see Fig. 18a, b, c, d, e, f):
a — Plane grasp
b — Pinch grasp
c — Cylindrical grasp
d — Spherical grasp
e — Interdigital grasp
f — Hook grasp
Mobility Assessment of the Lower Limb
Movement Assessment in the Hip Joint
Movements in the hip joint are evaluated with the patient in a horizontal position. When lying on their back, flexion is performed until the anterior surface of the thigh touches the anterior abdominal wall. Extension is assessed with the patient lying on their stomach, with the pelvis fixed.
Abduction varies within a wide range; on average, the extended thigh can be abducted to half of a right angle from the vertical axis of the body.
Rotation:
- During external rotation of the extended thigh, the outer edge of the foot can touch the horizontal surface.
- During internal rotation, the inner edge of the foot touches the horizontal surface.
When the thigh is flexed at a right angle:
- External rotation allows the heel to be placed on the opposite thigh.
- Internal rotation is minimal.
Extension-Flexion: 10°/0°/130° (see Fig. 19a, b, c).
Abduction-Adduction range in the hip joint: 50°/0°/40° (see Fig. 20a, b, c).
External-Internal rotation range in the hip joint: 50°/0°/50° (see Fig. 21a, b, c).
Movement Assessment in the Knee Joint
Movements are assessed with the patient in a lying position. When the popliteal surface touches the horizontal plane, the knee joint can be passively hyperextended, lifting the heel 5-10 cm above the surface. With maximum flexion, the heel can touch the buttock.
Extension-Flexion: 5°/0°/140° (see Fig. 22a, b).
 Fig. 22a
Fig. 22aLateral Movements in the Knee Joint
In the extended knee joint, lateral movements (abduction and adduction) are absent. When the knee is flexed and the lateral ligaments are relaxed, slight lateral movements are possible. Rotation in the knee joint is similar to lateral movements. Anterior-posterior displacement of the tibia relative to the femur is absent if the cruciate ligaments are intact, both in the extended and flexed knee.
Movement Assessment in the Ankle Joint
The neutral starting position: The foot is positioned relative to the tibia at a right angle, as in standing. Measurements are performed with the Achilles tendon relaxed, which is achieved by flexing the knee joint.
The ankle joint is a hinge joint. In plantar flexion, slight rotational and lateral displacements are possible but in very small amounts, which are difficult to measure. In the dorsiflexed position, the talus is fully locked in the mortise formed by the malleoli, making lateral displacements and rotation of the talus impossible.
Extension (dorsiflexion) — Flexion (plantar flexion): 20-30°/0°/40-50° (see Fig. 23a, b, c).
Assessment of Overall Mobility in the Tarsal and Tarsometatarsal Joints
The patient lies on their back with the knee extended. The leg is supported above the ankle joint. With full freedom of movement in all joints, the foot is first placed in a position of maximum adduction and supination (inversion), and then moved into a position of abduction and pronation (eversion).
- Adduction — 0°-45° and supination — 0°-35° (see Fig. 24).
- Abduction — 0°-30° and pronation — 0°-15° (see Fig. 25).
Movement Limitations in Joints
Various pathological processes—congenital, traumatic, inflammatory, and degenerative—can cause changes in joints, leading to:
1. Restricted joint mobility;
2. Increased range of motion, possibly resulting in pathological mobility;
3. Simultaneous manifestation of both restricted and increased mobility.
Types of Joint Mobility Restrictions
Mobility restrictions in a joint can arise from changes within the joint or outside it. The primary types of mobility restrictions include ankylosis, rigidity, and contractures.
- Ankylosis: Complete immobility of the affected joint. There are two types:
- Bony ankylosis: Absence of motion due to bony fusion of joint surfaces. Clinically characterized by a lack of movement and pain. Radiographically, the transition of bony trabeculae from one bone to the other can be seen.
- Fibrous ankylosis: The joint ends are connected by fibrous or scar tissue, holding the joint in a forced position. This presents with pain and limited, rocking movements. Radiographically, changes in the joint space are visible.
- Rigidity: Scar fusion of altered joint surfaces, closely related to fibrous ankylosis, but with slight rocking movements still possible.
- Contractures: These restrict movement in a joint in one plane and can be congenital or acquired.
Causes of Acquired Contractures
- Scarring after trauma, infections, or toxic damage to the joint and surrounding tissues.
- Reflex muscle tension due to prolonged limb immobilization.
- Muscle synergy disturbances in cases of paralysis, muscle, and tendon damage.
- Long-term limb immobilization.
Classification of Contractures by Genesis:
- Dermatogenic: Due to skin scar tension.
- Desmogenic: Caused by fascial or ligament shortening after deep trauma or chronic inflammation.
- Tendogenic: Develop from scarring and adhesions after tendon or sheath injury.
- Myogenic: Result from structural changes in muscles, loss of elasticity, or spastic contractions.
- Arthrogenic: Caused by changes in joints or the ligament-capsule apparatus.
- Neurogenic: Associated with diseases of the nervous system.
- Psychogenic (hysterical): Often occur following a hysterical seizure.
- Mixed contractures.
Classification of Contractures by Position:
- Flexion contractures: Restriction of extension.
- Extension contractures: Restriction of flexion.
- Adduction contractures: Restriction of abduction.
- Abduction contractures: Restriction of adduction.
- Pronation contractures: Restriction of supination.
- Supination contractures: Restriction of pronation.
- Combined contractures: Simultaneous restriction of several functions (e.g., flexion and extension).
Increased Range of Motion in Joints
Depending on the direction of additional movement, we distinguish between:
- Hyperextension, excessive abduction, adduction, rotation, etc.
Movements in atypical planes that do not match the form of the joint surface are also observed, particularly in joints that usually move in a single plane.
For example, when the anterior cruciate ligament (ACL) of the knee is injured, the anterior drawer sign is present (Fig. 26a), and with damage to the posterior cruciate ligament (PCL), the posterior drawer sign is seen (Fig. 26b).
Joint Instability
Joint instability can result from the following changes:
- Bony: Destruction of joint surfaces.
- Capsular-ligamentous: Tears or overstretching of the ligaments and capsule.
- Muscular: Loss of function in the muscles surrounding the joint.
- Neurological: Damage to the nerves that control joint stability.
Pathological Mobility at the Diaphyseal Level of Bones
Pathological mobility along the length of a bone is a pathognomonic symptom of a fracture.
Pathological mobility is also noted in:
- Non-union fractures: Elasticity or slight rocking movements with pain in the fracture area.
- Pseudoarthrosis (false joints): Marked pathological mobility or rocking movements without pain during examination or loading. The key radiological sign is the closure of the medullary cavity by an endplate.
- Bone defects: There is significant mobility between the bone segments.
Clinical Measurement of Limb Length
To accurately measure limb length, specific conditions must be followed:
- Measurements should be comparative (both the healthy and affected limbs should be measured).
- Symmetrical bony landmarks should be used as reference points.
The preliminary step in measurement is determining the limb axis (discussed earlier). Measurements are performed using a tape measure, which is pulled taut between the bony landmarks with sufficient force.
Lower Limb Length Measurement
For accurate measurement, the limbs should be positioned symmetrically. For the legs, this position must be parallel to the long axis of the body, as in a free-standing, upright position (neutral position). When lying on the back, the anterior superior iliac spines should be perpendicular to the body axis and at an equal level relative to the horizontal plane.
Pelvic asymmetry can be assessed by measuring the distance from the xiphoid process of the sternum to the anterior superior iliac spines (on the anterior surface) (see Fig. 27), and from the spinous process of one of the vertebrae to the posterior superior iliac spines.
Relative Length of the Lower Limb
The relative length of the lower limb is determined by measuring the distance from the anterior superior iliac spine to the apex of the medial malleolus of the tibia (see Fig. 28).
Anatomical (Absolute) Length of Segments
Thigh: The length is measured from the apex of the greater trochanter to the knee joint line (see Fig. 29).
Lower leg: The length is measured from the knee joint line to the apex of the lateral malleolus (see Fig. 30).
Measurement of Upper Limb Length
For upper limb measurement, the arms should be positioned parallel to the torso, with the lower angles of the scapulae or the acromial processes at the same level.
Shoulder width is measured from the outer edge of the acromion to the edge of the sternal notch of the manubrium (see Fig. 31).
Relative length of the upper limb is determined by measuring the distance from the acromioclavicular joint to the apex of the styloid process of the radius (see Fig. 32).
Arm (Humerus): The anatomical (absolute) length is measured from the greater tubercle of the humerus to the lateral epicondyle of the same bone (see Fig. 33).
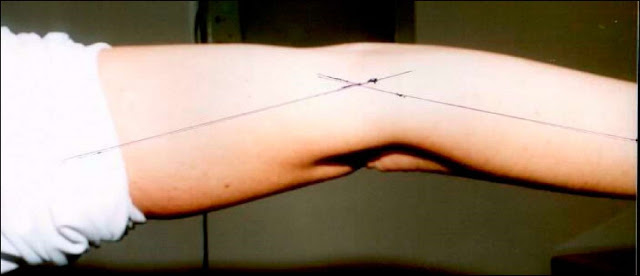
Forearm: The anatomical (absolute) length is measured from the apex of the olecranon to the apex of the styloid process of the ulna (see Fig. 34).
Types of Limb Shortening (Lengthening)
- True (anatomical) shortening (lengthening): This is identified when segmental measurement reveals a shortening or lengthening of one of the bones compared to the symmetrical segment of the healthy limb. Causes may include epiphyseal plate damage with delayed bone growth, displacement of fracture fragments, improperly healed fractures, etc. Anatomical lengthening can occur due to excessive growth of the epiphyseal plate.
- Relative shortening (lengthening): This occurs due to changes in the positioning of joint segments (e.g., dislocations or subluxations).
- Functional shortening: Defined as the distance from the heel to the floor when the line connecting the anterior superior iliac spines is horizontally aligned. It is determined using wedges and consists of the sum of anatomical and relative shortening.
Circumference Measurement of Limb Segments and Joints
In cases of muscle atrophy, joint effusion, or edema, measuring the circumference of the affected and healthy limbs allows for tracking changes over time. The circumference is measured at symmetrical locations at a specific distance from bony landmarks. For example, the circumference of the right thigh, 20 cm proximally from the knee joint line, is 52 cm (see Fig. 35), while the left thigh at the same level is 50 cm. Thus, there is a reduction in the left thigh circumference by 2 cm.
Measuring Segment Width and Thickness
The width and thickness of the affected and healthy limb segments are measured using a caliper.
Muscle Strength Assessment
A range of musculoskeletal deformities is caused by disruptions in normal muscle synergy, reduced or absent function of specific muscle groups, or uneven muscle strength. In such cases, it is essential to assess the muscle strength of the limb, as this information is crucial for developing an effective treatment plan.
Muscle strength is assessed using active movements against resistance provided by the physician. Muscle strength is graded on a six-point scale:
1. 100% - 5 points (Normal): Full range of motion with the limb’s own weight and external resistance.
2. 75% - 4 points (Good): Full range of motion with the limb’s own weight and reduced external resistance.
3. 50% - 3 points (Satisfactory): Full range of motion with the limb’s own weight only.
4. 25% - 2 points (Poor): Full range of motion with external assistance.
5. 5% - 1 point (Very Poor): Muscle contraction is palpable, but no joint movement occurs.
6. 0% - 0 points (None): Complete absence of muscle function.
To ensure objective control of muscle strength, devices such as dynamometers and myotonometry can be used. For a comprehensive analysis of the musculoskeletal system’s functional status, complex biomechanical studies with specialized equipment may be employed.
Radiological Diagnosis
Radiological imaging (X-ray or Puluy’s rays) plays a significant role in diagnosing musculoskeletal injuries and diseases and is used at various stages of diagnosis, during treatment, and post-treatment.
Key principles of radiographic imaging:
1. The affected area should be centered in the image.
2. For injuries to the diaphysis of long bones, the radiograph should include two adjacent joints, while for fractures of the tibia and forearm bones, the entire limb segment, including both joints, should be captured.
3. Radiographs should be taken in at least two perpendicular projections. Oblique or axial projections and imaging of the symmetrical area may be used if indicated.
4. The radiographs must be of high quality.
Changes in Bone and Joint Shape
Bone and joint deformities can be congenital or acquired. Radiologically, the following typical bone changes may be observed:
- Aplasia: Congenital absence of part or all of a bone due to developmental abnormalities.
- Hypoplasia: Delayed or arrested endochondral growth of the bone.
- Hyperplasia: Accelerated endochondral and periosteal bone growth.
- Atrophy: Decrease in bone size due to reduced macroscopic structure.
- Osteolysis: Local bone resorption, where bone becomes thinner or completely disappears.
- Usure: Small marginal defect on the bone's outer contour.
- Osteoporosis: Decrease in the number of bone trabeculae per unit volume, leading to increased radiolucency.
- Osteopenia: Physiological reduction in bone mass per unit volume.
- Osteosclerosis: Thickening and increased number of trabeculae, resulting in bone densification.
- Hyperostosis: Excessive periosteal growth in bone thickness.
- Hypostosis: Reduced periosteal thickening, causing the bone to become thin and deformed.
- Periostosis: Formation of new bone layers around the diaphysis due to periosteal bone growth.
- Osteophytes: Small, localized periosteal bone growths.
- Exostoses: Large, localized periosteal bone growths.
Key Stages of Radiograph Analysis
1. Evaluation of bone and joint position, shape, and size:
- Long bones may deform at the diaphysis, metaphysis, or epiphysis. Fracture displacement may occur along the bone's length, width, axis, or angle. In children, "greenstick" fractures show no displacement. The width of the radiographic joint space is determined by the articular cartilage. Misalignment of articulating surfaces can result in dislocation or subluxation.
- Dislocation: Characterized by a complete loss of contact between joint surfaces.
- Subluxation: Partial loss of contact with disruption of articulation and joint space uniformity.
- Auxiliary lines, such as Shenton’s line or Calve’s line, are often used to detect subluxations and dislocations.
- Joint space widening: Seen in hemarthrosis or effusion.
- Joint space narrowing: Occurs with cartilage destruction or degenerative-dystrophic changes (e.g., osteoarthritis or aseptic necrosis).
2. Changes in external bone and joint contours:
- Bone contours may be altered by inflammatory, degenerative, or neoplastic processes in the bone or adjacent soft tissues.
- Exostoses: Often result from developmental abnormalities.
- Osteophytes: Arise from degenerative-dystrophic or inflammatory processes.
3. Changes in bone internal structure:
- The thickness of the diaphyseal cortex, the diameter of the medullary canal, and the size of the ossification centers in children should be assessed. The internal structure of cancellous bone is characterized by the arrangement of bone trabeculae, which depends on functional load. Correct or abnormal alignment of these trabeculae should be determined.
- Osteolysis and osteoporosis manifest as increased radiolucency due to bone mass loss.
- Osteosclerosis, on the other hand, results in bone densification and reduced radiolucency.
- Radiomorphometric analysis of bone structure (e.g., femur or vertebrae) helps assess changes in bone density.
Osteoporosis
Osteoporosis is the reduction of bone mass per unit volume. On radiographs, it appears as increased transparency, thinning of the cortical layer, widening of the medullary canal, and more defined cortical layer contours. Types of osteoporosis include:
- Spotted osteoporosis: Appears as small or large areas of radiolucency.
- Diffuse or homogeneous osteoporosis: Develops after the spotted stage.
Localized osteoporosis affects one area, while regional osteoporosis involves an entire limb segment or body region.
- Regional osteoporosis can result from immobilization or reflex processes following trauma (Sudeck's syndrome).
Osteosclerosis
Osteosclerosis is the densification of bone structure, manifested on radiographs as the disappearance of the typical bone pattern. The bone becomes denser and less penetrable by X-rays.
Radiological (Puluy) Densitometry
Dual-energy X-ray densitometry is used to measure bone density. Specialized software accurately determines bone mineral density (BMD) in various skeletal regions (e.g., vertebrae, femur) and monitors changes over time through repeated studies.
Soft Tissue Changes
Soft tissues can be visualized on radiographs using "soft" radiation techniques. Shadows in soft tissues are commonly observed during inflammatory processes, leading to tissue infiltration. Gas inclusions in soft tissues are seen in anaerobic infections, particularly in cases of gas gangrene.
A unique group of conditions includes ossifying diseases, such as:
- Ossifying myositis,
- Heterotopic ossifications.
These pathological conditions are characterized by the appearance of spots in the muscles or other areas not typically associated with bone tissue. These spots eventually ossify, resembling bone tissue on radiographs.
Radiographic examination of soft tissues is crucial for detecting foreign bodies.
X-ray Television Imaging
This method uses an image intensifier (I.I.) and television system to monitor diagnostic procedures during surgery. The advantage of this method is the significantly reduced radiation exposure to both the patient and medical personnel compared to conventional fluoroscopy. The image can be saved as a radiograph on photographic paper.
Contrast Methods
Contrast agents are commonly used to visualize anatomical structures not visible on standard radiographs:
- Arthrography: This method involves injecting a contrast agent into the joint cavity to obtain an image of the joint. Double contrast techniques involve injecting a contrast agent (e.g., Urografin, Verografin) along with air or oxygen.
- Bone Scintigraphy: This radionuclide imaging method visualizes bone tissue. Phosphate compounds labeled with technetium are injected intravenously. This method helps evaluate blood flow and metabolic activity in the bone.
- "Cold zones" (areas of low radionuclide uptake) are characteristic of aseptic necrosis or bone infarction.
- "Hot zones" (areas of increased radionuclide uptake) are seen in osteomyelitis, tumors, and metastases.
Computed Tomography (CT)
Computed Tomography (CT) was first clinically applied in 1972. The method is based on mathematical data processing to obtain cross-sectional images of tissues. Each tissue segment has its X-ray absorption coefficient, measured in Hounsfield units (HU). CT provides detailed images of intra-articular, extra-articular injuries, and tumors extending beyond the bone.
Magnetic Resonance Imaging (MRI)
Magnetic Resonance Imaging (MRI) is a modern diagnostic method offering many advantages. Unlike CT, MRI does not use ionizing radiation; instead, it uses a magnetic field to generate images of tissues. The hydrogen protons in the body's tissues change their orientation under the influence of a magnetic field and return to their original state after the magnetic field is turned off. These changes are recorded and processed to produce images in frontal, sagittal, axial, or oblique planes.
Advantages of MRI:
- Detects soft tissue edema.
- Clearly identifies ligament and tendon injuries, differentiating between tears and sprains.
- Useful for early diagnosis of bone tumors and evaluating their spread (intramedullary or extramedullary).
- Visualizes nerves, blood vessels, joint capsules, ligaments, and pathologies in the epidural space.
MRI is also valuable for differentiating between fibrotic changes, hematomas, abscesses, metastases, leukemia, and other pathological conditions in soft tissues.
Example: MRI of the shoulder joint (see Fig. 37).
Subacromial-Subdeltoid Bursitis: Inflammation of the subacromial-subdeltoid bursa, which may result in pain and restricted movement in the shoulder.
Lipoma: A benign tumor composed of adipose tissue, usually soft and movable upon palpation.
Avulsion Fracture of the Greater Tuberosity of the Humerus: This occurs when a fragment of the greater tuberosity is torn away from the humerus, typically due to trauma or a strong muscle contraction.
Contraindications for MRI include the presence of metallic foreign bodies in the tissues, which can pose a risk during imaging.
Avulsion Fracture of the Greater Tuberosity of the Humerus: This occurs when a fragment of the greater tuberosity is torn away from the humerus, typically due to trauma or a strong muscle contraction.
Contraindications for MRI include the presence of metallic foreign bodies in the tissues, which can pose a risk during imaging.
Ultrasound Examination (Ultrasonography)
Ultrasound has become an invaluable tool in orthopedic sonography. Austrian orthopedic specialist K. Ogg significantly contributed to its development in 1980 by introducing ultrasound for diagnosing congenital hip dysplasia and congenital hip dislocation. Since then, ultrasound has been widely used for diagnosing and monitoring musculoskeletal diseases in both children and adults.
Arthrosonography is particularly useful in diagnosing inflammatory joint diseases before bone destruction occurs.
Fig. 38: Ultrasound of both knee joints in rheumatoid arthritis (RA) demonstrates characteristic changes associated with inflammation.
Ultrasound Findings in Rheumatoid Arthritis (RA)
Synovial membrane thickening: An increase in the thickness of the synovial lining, which is commonly observed in inflammatory conditions such as rheumatoid arthritis.
Synovitis: Inflammation of the synovium, resulting in joint swelling and effusion, which can be detected via ultrasound as anechoic or hypoechoic fluid within the joint space.
Synovial proliferation: The overgrowth of synovial tissue, often seen in chronic inflammatory conditions like RA, where the synovium becomes hyperplastic, potentially leading to joint destruction.
Доплерографічна УЗД дозволяє оцінити рівень кровообігу в м’яких тканинах.
Fig. 39: Blood Flow in the Synovial Membrane of the Knee Joint in Rheumatoid Arthritis (RA)
In rheumatoid arthritis (RA), increased blood flow can be detected in the synovial membrane using Doppler ultrasound. This increased vascularization is a hallmark of active inflammation and can be visualized as areas of hyperemia (increased blood flow) within the synovium.
Hypervascularity: Doppler imaging shows elevated blood flow in the inflamed synovial membrane, which is indicative of ongoing inflammatory activity.
Monitoring synovial blood flow in RA is essential for assessing the severity of inflammation and guiding therapeutic decisions, as increased vascularity often correlates with disease activity and joint damage.

Ultrasound in the Diagnosis of Soft Tissue Injuries and Diseases
Ultrasound is a highly effective tool for diagnosing soft tissue injuries and conditions affecting muscles, tendons, and ligaments. The benefits of using ultrasound in musculoskeletal diagnostics include real-time imaging, non-invasiveness, and the ability to visualize soft tissues that may not be apparent on X-rays.
Key soft tissue pathologies identified with ultrasound include:
- Muscle injuries: Tears, strains, and contusions can be visualized, showing discontinuity, fluid collections, or hematomas within the muscle fibers.
- Tendon pathology: Tendon tears, tendinitis, and tendinosis are commonly diagnosed using ultrasound, which allows the visualization of changes in tendon structure, swelling, and fluid accumulation around tendons.
- Ligament injuries: Sprains, partial, or complete ligament tears can be easily identified. Ultrasound provides detailed images of the ligament's integrity and any surrounding inflammation or effusion.
The use of ultrasound-guided procedures, such as injections or aspirations, enhances the accuracy and safety of therapeutic interventions in soft tissue injuries.
Fig. 40: Ultrasound Diagnosis of Long Head of Biceps Tendon Injury (m. biceps brachii)
In this ultrasound image, injury to the long head of the biceps brachii tendon is evaluated. Key findings typically observed during ultrasound examination of this region include:
- Tendon rupture: A discontinuity or complete tear of the tendon fibers may be visible. In a complete rupture, the tendon retracts and may not be visible in its normal anatomical location.
- Tendinosis or tendinitis: This can appear as swelling or thickening of the tendon with hypoechoic (dark) regions due to inflammation or degenerative changes.
- Effusion or fluid collection: Fluid accumulation around the tendon sheath indicates inflammation or injury.
Ultrasound is a valuable tool in assessing tendon integrity, especially for diagnosing partial or complete tears of the long head of the biceps brachii tendon.
Fig. 41: Ultrasound Diagnosis of Rotator Cuff Injury
Ultrasound imaging is highly effective for diagnosing injuries to the rotator cuff of the shoulder. Common findings in rotator cuff pathology may include:
- Tendon tears: Partial or full-thickness tears of the supraspinatus, infraspinatus, or other components of the rotator cuff can be visualized as gaps or disruptions in the tendon fibers.
- Tendinosis: Chronic degenerative changes in the tendons, visible as thickening or hypoechoic areas within the tendon.
- Fluid accumulation: Fluid around the rotator cuff, indicating bursitis or joint effusion, may be detected.
- Calcifications: Calcific tendinitis can present as hyperechoic (bright) deposits within the tendons.
Ultrasound and Early Detection of Periosteal Pathology
Ultrasonography is extremely valuable for detecting pathological changes in the periosteum and fluid accumulation beneath it, especially during the so-called “X-ray negative” period. During this early stage of inflammatory or neoplastic processes, traditional X-rays may fail to detect the initial changes. Ultrasound allows for the early diagnosis of conditions, enabling timely treatment before more pronounced bone alterations occur.
Ultrasound Densitometry of the Calcaneus (Heel Bone)
Ultrasound densitometry is widely used to assess bone tissue, particularly for detecting osteoporosis or osteosclerosis. It is a non-invasive, quantitative method that measures bone mineral density (BMD).
Ultrasound Densitometry (Ultrasonometry)
This modern method measures bone density based on the speed of sound waves traveling through the bone and the broadband attenuation of ultrasound waves within bone tissue. From these parameters, the computer calculates an integrated measure of trabecular bone health, known as the Stiffness Index. This index is crucial for determining the degree of osteoporosis, making ultrasound densitometry an important tool for diagnosing bone metabolism disorders.
Electromyography (EMG)
Electromyography (EMG) is a technique used to record the fluctuations of biopotentials generated by muscles, allowing for an assessment of the functional state of both muscles and the neuromuscular system. EMG can help determine whether changes in electrical activity are due to nervous system impairment or muscle pathology. EMG data are crucial for refining a topical diagnosis and objectifying pathological processes. For example:
- Reflex changes in muscle tone are characterized by a slight increase in the amplitude of frequent, rapid oscillations.
- In muscle hypotrophy, there is a reduction in the amplitude of biopotentials.
- In cases of flaccid paralysis, EMG reveals the so-called "bioelectrical silence", indicating the absence of electrical activity.
Thermography
Thermography is a method that records the thermal radiation emitted by the human body in the infrared range. This technique creates a "thermal image" of the body's segments and is used to assess peripheral blood flow, diagnose arthritis, osteomyelitis, and tumors. Thermal imaging diagnostics (radiothermography) measures the temperature of both surface and deep tissues based on their intrinsic radiation, which aids in evaluating blood flow and inflammatory processes.
Laboratory Investigations
Laboratory tests play a key role in identifying the nature of diseases, aiding in differential diagnosis, and confirming orthopedic conditions. Continuous laboratory monitoring is essential for tracking the progression of the pathological process and the effectiveness of treatment.
Biochemical Tests
Biochemical investigations are divided into:
1. Routine tests: These include measuring liver enzymes, C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), calcium, phosphates, oxyproline, creatinine, as well as 24-hour urinary excretion of calcium, phosphates, and oxyproline.
2. Additional tests: These involve assessing collagenase activity, alkaline phosphatase, and various hydroxyproline fractions.
3. Highly specialized tests: These include measuring hormone levels, glucosaminoglycan fractions, and employing radioimmunoassays and other advanced technologies, typically conducted in osteology and nephrology centers.
Synovial Fluid Analysis
Synovial fluid analysis is vital for the differential diagnosis of arthritis and arthrosis and involves both physical and chemical investigations, such as:
- Viscosity determination,
- Mucin clot formation evaluation,
- Biochemical analysis, including protein concentration, glucose levels, hyaluronic acid, and chondroitin sulfates.
Sources:
1. Андрианов В.П., Байров Г.А. та ін. Заболевания и повреждения позвоночника у детей и подростков. — М.: Медицина, 1985. — 256 с.
2. Битхем У.П., Палей Г.Ф. та ін. Клиническое исследование суставов. — М.: Медицина, 1970. — 187 с.
3. Бур’янов О.А. зі співавт. Особливості клінічного обстеження плечового суглоба у спортсменів. // Літопис травматології та ортопедії. — К., 2002 (3-4). — С. 71-75.
4. Граф Р., Фаркас П. та ін. Ультрасонография в диагностике и лечении дисплазии тазобедренных суставов у детей. — Вильнюс, 2001. — 42 с.
5. Кашуба В.А. Биомеханика осанки. — К.: 2002. — 278 с.
6. Казарезов М.П. Контрактуры. — М.: 2002. — 255 с.
7. Крись-Пугач А.П. зі співавт. Обстеження та діагностика опорно-рухових розладів у дітей. — Київ-Хмельницький, 2002. — 216 с.
8. Линденбратен Л.Д., Королюк И.П. Медицинская радиология и рентгенология. — М.: Медицина, 1993. — 560 с.
9. Лябах А.П. Клінічна діагностика деформацій стопи. — К.: ЗАТ «Атлант ЮЕмСі», 2003. — 110 с.
10. Маркс В.О. Ортопедическая диагностика. — Минск: 1978. — 508 с.
11. Николаев Л.П. Руководство по биомеханике в применении к ортопедии травматологии и протезированию. — К.: 1950. — 187 с.
12. Орнштейн Е., Войня А. Семиотика и диагностика в травматологии и ортопедии. — Кишинёв, 1992. — 450 с.
13. Поворознюк В.В., Подрушняк Е.П., Орлов Е.В. Остеопороз на Украине. — К.: 1995. — 48 с.
14. Смiян С.І., Масик О.М. Сучасна діагностика змін мінеральної щільності кісткової тканини з використанням методу двофотонної рентгенівської денситометрії (методичні рекомендації). — Тернопіль: «Укрмед», 2001. — 24 с.
15. Франк Ю., Рунге Г. Остеопороз. — М.: Медицина, 1995. — 300 с.
16. Языков Д.К. Дифференциальная диагностика в клинике травматологии и ортопедии. — М.: Медгиз, 1963. — 124 с.
17. Янсон Х.А. Биомеханика нижней конечности человека. — Рига: Зинатне, 1976. — 356 с.
18. Burk Jr. DL, Karasick D, Kurtz AB, et al. Prospective Comparison of MR Imaging with Arthrography, Sonography, and Surgery. AJR 153: 87-92, 1989.
19. Frank A., Pettrone. Athletic Injuries of the Shoulder. — 1995. — 390 p.
20. Peh WCG, Cassar-Pullicino VN. Magnetic Resonance Arthrography: An Update. Clin Radiol, 1999: 54: 575-587.
21. Pusse O. Atlas of Examination Standard Measurements and Diagnosis in Orthopaedics and Traumatology. Stuttgart: 1987. — 582 p.
22. Stoller DW, Wolf EM. The Shoulder. In: Stoller DW, ed. Magnetic Resonance Imaging in Orthopaedics and Sports Medicine. 2nd ed. — Philadelphia: Lippincott-Raven, 1997. — 597-742.
23. Матеріали кафедри травматології та ортопедії НМУ ім. О.О. Богомольця.
If you find an error, please highlight the text fragment and write about it in the comments.